What are Hemorrhoids?
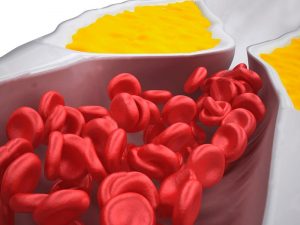
Hemorrhoids (also known as piles) are veins around the anus or lower rectum that have become swollen and/or inflamed. The rectum is the last few inches of the colon and connects to the anal canal. Piles are most commonly the result of excess strain occurring during a bowel movement. There are two types of hemorrhoids:
- External hemorrhoids: These veins form underneath the skin around the anus. Because external hemorrhoids are covered by an extremely sensitive skin, they are the more painful form of piles.
- Internal hemorrhoids: These veins form in the lining of the anus and lower rectum. These piles are covered in a protective lining called mucosa. Internal hemorrhoids are not sensitive to touch, pain, stretching or temperature because of this lining.
Men and women are both equally susceptible to developing piles, and about one in 20 Americans are affected. Almost half of adults aged 50 or older have this condition.
Causes
- Sitting on the toilet for long periods of time.
- Strain during bowel movements.
- Chronic constipation or diarrhea.
- Eating high-fiber
- Pregnancy.
- Lifting heavy objects.
Symptoms
Piles are the most common cause of anal symptoms, but they are not the only cause. The same symptoms can be a sign of digestive tract problems, bowel diseases or colon cancer.
Possible symptoms for external hemorrhoids include:
- Anal itching.
- One or more hard, tender lumps near the anus.
- Anal aches or pains, particularly when sitting.
The primary symptoms of internal hemorrhoids are painless rectal bleeding and prolapse. These piles are categorized by their degree of prolapse (hemorrhoidal tissue that falls through the anal opening).
- Grade one: No
- Grade two: Prolapse that goes back in on its own.
- Grade three: Prolapse that must be pushed back in by the patient.
- Grade four: Prolapse that cannot be pushed back in by the patient (usually very painful).
The grade of hemorrhoid determines the method of treatment. Consult your doctor if symptoms have not subsided after a week of at-home treatment. Excess straining, rubbing or cleaning around the anus can exacerbate symptoms.
Hemorrhoid Complications
In most cases this condition doesn’t cause major problems. Only 5 per cent of people in the United States seek medical care for their hemorrhoids. Major complications can include:
- Blood clots (external piles).
- Skin tags (extra skin after blood clot dissolves).
- Sore infections.
- Strangulated piles (occurs when the muscle around the anus cuts off the blood supply to an internal pile).
- Anemia.
Hemorrhoids Treatment
Symptoms and issues that arise from external and internal piles can differ and therefore require different treatments. However, both can usually be treated at home.
At-Home Solutions:
- A warm sitz bath several times a day for about 10
- Place an ice pack on the affected area to reduce swelling.
- Spend shorter periods of time on the toilet.
- Make bowel movements as soon as you get the urge rather than holding them in.
- Make lifestyle changes to ensure softer stool (exercise, drink water, change your diet).
Hemorrhoids Diet
Doctors may recommend to people suffering from piles that they make dietary changes to soften the stool. Suggested foods/beverages are all rich in fiber and include:
- Whole-wheat spaghetti.
- Oat bran muffins.
- Bran.
- Pears with the skin.
- Apples with the skin.
- Stewed prunes.
- Green peas.
- Cooked collards.
- Baked potatoes.
- Kidney beans.
- Pinto beans.
In addition to high-fiber foods, drinking lots of water, fruit juices and clear soups can help with digestion. Foods to avoid that can cause chronic constipation include cheese, chips, fast food, ice cream, meat, prepared foods and processed foods.
Doctor-Administered Treatments:
- Hemorrhoids Surgery (hemorrhoidectomy): Fewer than 10 per cent of all patients evaluated with symptomatic hemorrhoids will require surgical management. This treatment option is used for extremely severe piles that are prolapsing. Patients are put under anesthesia and a surgeon removes the hemorrhoidal tissue. After the procedure the surgeon may perform a “stapled hemorrhoidopexy” to decrease postoperative pain. During this operation a stapling device is used to remove tissue on the upstream of the piles, thus pulling them upward to their normal position. The tissue is then stapled into place and falls out over time. Although this method is newer, it has been shown to be safe and to shorten recovery time
- Rubber Band Ligation: Also referred to as banding, this procedure uses a small rubber band. The band is placed around the bottom of the pile inside the rectum, cutting off circulation. Within seven to 10 days the hemorrhoid begins to decay and falls off, along with the band. A scar then forms and prevents further bleeding or prolapse. Recovery time for banding is quite fast and patients can expect to return to daily activities immediately. This method of treatment can work on grade one and two piles.
- Sclerotherapy: This treatment option involves an injection. Chemical irritants are infused into the piles, causing the blood vessels inside to shrink. Sclerotherapy is a very easy and painless procedure with little complication. It can take several sessions before the patient experiences active hemorrhoid relief.
- Thrombosed External Hemorrhoids: External hemorrhoids can be treated with an excision if patients see a doctor within the first 24 hours of pain. If not, the pile will go away on its own and surgery is not recommended. Warm baths can help sooth
If you have experienced any symptoms associated with hemorrhoids, see your doctor immediately before self-treating, as there is the risk they are symptoms of a more serious condition. Your healthcare professional will perform a formal physical exam or digital rectal exam to determine a diagnosis. As with any condition, make sure the doctor treating you has your complete medical history.